When advertising professional Caroline Tchakerian, 25, encounters a friend about to start treatment with Ozempic, a medication for diabetes also used for weight loss, she avoids mentioning the side effects she experienced while using the injectable medication.
+ Can diabetes medications be used for weight loss? What do experts say?
“I felt so nauseous. I would wake up feeling sick, sweating cold, and couldn’t sleep anymore. Then, I had a stomach ache that got so bad I had to go to the emergency room,” says the advertising professional.
Despite the side effects, she says she doesn’t want to discourage others interested in the medication. “It’s a complicated situation because, even with the side effects, I lost almost 10 kilos, and everyone thinks that’s great. [To] several friends who are just starting now, I warn them that they might feel unwell, but sometimes it seems like it’s because I’ve already ‘made it’ and I don’t want others to lose weight too,” she says.
The advertising professional states that she doesn’t regret using the medication, which was prescribed by an endocrinologist because she was above her ideal weight and had fatty liver disease, also known as fat in the liver. Despite this, she reports being concerned about its indiscriminate use by colleagues and acquaintances, almost always without the same medical supervision. “Everyone is using it,” the young woman adds.
In São Paulo, pharmacies in the expanded center report difficulties in keeping the product in stock, which is manufactured by the Danish laboratory Novo Nordisk. However, the ‘frenzy’ for using Ozempic is not exclusive to Brazil. In the United States and Australia, the rampant demand has caused the medication to disappear from shelves and become a topic in major newspapers.
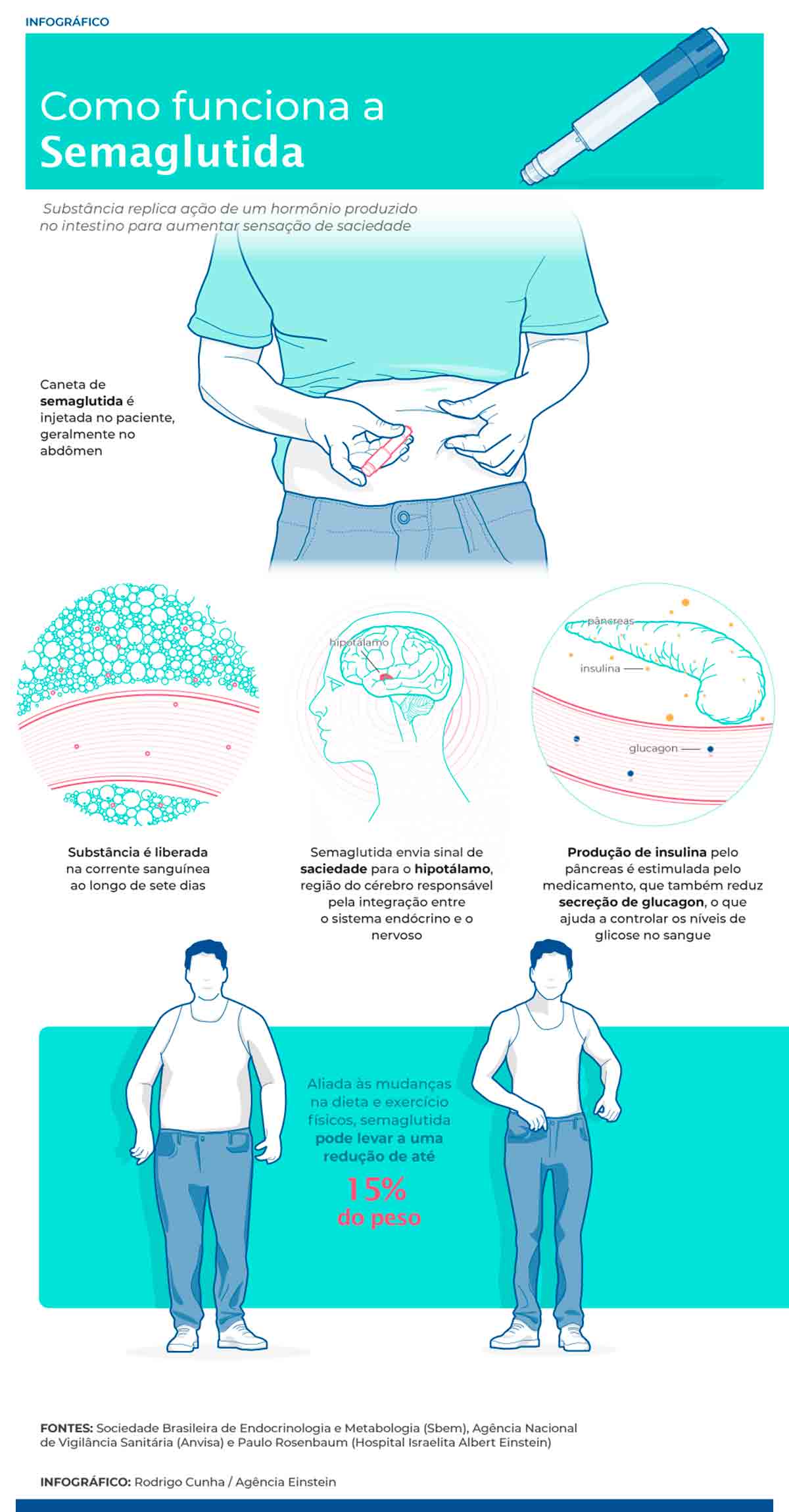
The medication contains semaglutide as its active ingredient, a synthetic hormone that helps control blood glucose levels and signals the brain to feel full. It mimics the effects of GLP-1, a natural hormone produced in the intestine.
Its intended use, according to the package insert, is for the treatment of diabetes, but the medication has been prescribed by doctors off-label (not included in the insert) for weight loss. Endocrinologist Paulo Rosenbaum from the Albert Einstein Hospital explains that the use of the obesity medication is safe and has been extensively studied by scientists. However, treatment needs to be supervised by a doctor to be safe.
“If properly indicated, medications based on semaglutide are a revolution in the field of endocrinology. But the current demand for Ozempic is dangerous because, no matter how safe the medication is, it cannot be used without supervision,” says Rosenbaum.
Transitory Side Effects
The specialist explains that side effects like those reported by the advertising professional are common at the beginning of treatment, but usually improve after a few weeks. However, he reminds us that for about 10% of patients, the side effects do not cease, and other alternatives need to be sought.
“Research shows that about 10% of patients may experience more side effects and sometimes will not be able to tolerate the medication. That’s why it’s important to have medical supervision. The vast majority tolerate it well, experience side effects, but they are transitory and tend to decrease after one or two months,” explains the endocrinologist.
Tássia Gomide Braga, the medical manager at Novo Nordisk, which manufactures Ozempic, also emphasizes that side effects are more common at the beginning of treatment. The endocrinologist reminds us that, for now, the medication is only approved by the National Health Surveillance Agency (Anvisa) for diabetes – the prescription for weight loss is off-label, meaning it’s done at the doctor’s own risk.
“The majority of events are mild to moderate in severity and occur transitorily, lasting for a few days or a few weeks. The need to discontinue the medication due to adverse events is low,” states Braga. She explains that adverse effects tend to occur during the initial use of the medication or when there is an increase in the medication dose. “The patient should seek guidance from their doctor to minimize them,” adds the medical manager of the company.
It is still unclear what causes the side effects associated with semaglutide. According to the doctor at Novo Nordisk, one of the mechanisms of action of GLP-1 analog medications – a category that includes Ozempic – is the “transient decrease in the rate at which the stomach empties after a meal, which may be related to some of these effects.”
To avoid adverse reactions, it is common for doctors to prescribe the medication with a dosage ramp-up. Thus, treatment starts with a lower dose, which is gradually increased until it reaches what is considered ideal for each patient.
“A person might start with 0.25mg per week, while the dosage of one unit of the product is four times higher, at 1mg per week. During this ramp-up period, they may either have a quick response or may not notice any effect at all,” explains Rosenbaum, the endocrinologist at Einstein. The pharmaceutical industry doctor states that properly adhering to the dosage ramp-up minimizes the risk of side effects and can be adapted to the patient’s tolerability.
The ramp-up was the solution to the side effects experienced by executive Priscila Simões, 50, who started treatment with Ozempic in April 2022. In the first three months, she found it very difficult to use the medication, which was prescribed by an endocrinologist to treat overweight and fatty liver disease.
“I had a lot of nausea, diarrhea, stomach pain; it was horrible. You could tell it was really a gastrointestinal issue. In the beginning, I said we lose weight because we can’t eat due to the nausea,” recalls Simões.
The situation improved after she scheduled a new appointment with her doctor and was advised to reduce the dosage, increasing the amount each week until reaching the indicated dose.
“When I did that, it improved a lot. Now, I can take the prescribed dosage and eat normally, without nausea, but in much smaller amounts. I still eat the things I used to eat, but I’m significantly reducing the portion size,” explains the executive.
Diet During Treatment
Reducing portion sizes is one of the recommendations from Novo Nordisk to lessen side effects during treatment with Ozempic. Avoiding fatty foods and alcoholic beverages can also help control the nausea caused by the medication.
“In general, eating smaller portions at meals, stopping when feeling satisfied, avoiding fried and overly fatty foods, staying well hydrated throughout the day, and avoiding alcohol are actions that can minimize these side effects,” explains Braga.
Another alternative may be prescribing anti-nausea medications or gastric protectors for patients experiencing gastrointestinal effects, according to endocrinologist Rosenbaum. “There are a few possibilities, such as prescribing anti-nausea medications that the patient can take before meals, or even prescribing gastric protectors to avoid reflux,” explains the doctor.
“People need to be well-informed, because otherwise, we end up seeing patients who could benefit from the treatment but give up because they didn’t have guidance to avoid some effects,” evaluates the doctor.
Indiscriminate Use
The indiscriminate use of Ozempic without medical supervision worries entities and specialists in the field. In January, the Brazilian Society of Endocrinology and Metabolism (Sbem) issued a statement warning that, like any other medication, semaglutide “requires medical supervision and should only be used under prescription.”
The rampant demand has even affected patients with diabetes, who cannot find the medication in pharmacies in São Paulo. “There is a shortage of medicine for those who need it, for those who have diabetes, and that’s a shame. With this trend on social media, it has become crazy. There are people who shouldn’t even be using Ozempic but are doing so, experiencing all these side effects, and it’s lacking for those who actually need it,” evaluates Rosenbaum.
Even patients who have used the medication with professional guidance express concern about the craze for injectable semaglutide.
“I know a lot of people using it, but most of my friends are not following up with an endocrinologist. I see a lot of irresponsible posts
on TikTok teaching people how to use it, but no one talks about the tests that need to be done before treatment,” says advertising professional Tchakerian.
“I feel like there is a trend; a lot of people came to tell me they were going to take it too, and I always tell them to ask for medical guidance. I did all of this with a prescription, but it’s a medication that people are taking indiscriminately,” agrees executive Simões.
Rebound Effect
One of the risks of indiscriminate use is the so-called rebound effect, which occurs when the weight lost during treatment is regained once the patient stops using the medication. In some cases, the weight gain can even be greater than the amount lost previously.
“When you use it without guidance, you can experience a rebound effect, an unusual weight gain, especially when use is stopped without an action plan,” explains Rosenbaum. “If a person doesn’t change their lifestyle or exercise, they will gain all the weight back when they stop the medication,” adds the endocrinologist.
To avoid gaining weight again, experts recommend that the discontinuation of the medication be done gradually and, of course, accompanied by dietary changes and regular physical exercise.
“I am concerned about the rebound effect because I don’t want to regain the weight I lost, but I also don’t intend to take the medication for the rest of my life. I will try to maintain my weight with other mechanisms, through physical activity and diet,” says Simões.
Her strategy is similar to that of the advertising professional, who stopped using the medication in December after a series of side effects.
“When I stopped the medication and my hunger returned to normal, I felt like it was dragon hunger because I used to eat so little. Ozempic made me develop an important habit of eating less and exercising. Now, I continue going to the gym and have tried to adjust my diet, but I’m much hungrier than before,” explains Tchakerian.
As the cost of the medication is high—at the dosage indicated by endocrinologists, expenses can reach around R$ 1,000 per week—the alternative adopted by the advertising professional was to redirect her investment. “Now, the money I spent on the medication, I’m spending on a personal trainer. It’s not the same, but I’m trying to have more control,” concludes Tchakerian.
Source: Agência Einstein
The post Diabetes Medication Used for Weight Loss Has Adverse Side Effects appeared first on Agência Einstein.

